Diabetic Eye Care
Diabetes is the leading cause of blindness in young Americans. Diabetic Retinopathy is the most common sight threatening problem. There are other eye diseases diabetics suffer that contribute to visual limitation such as nerve palsies, optic nerve inflammation and early cataract formation. Diabetics should have yearly eye examinations.
Diabetic retinopathy is a disease of the retina, which is the tissue lining the back of the eye that turns light images into visual signals sent to the brain. The longer you are a diabetic and the less controlled your blood sugar is, the more likely you will develop diabetic retinopathy. Diabetic retinopathy affects the retina in two ways: proliferative retinopathy, which has new abnormal blood vessels growing and non-proliferative retinopathy (without new blood vessels growing) that can lead to swelling of the retina. Both forms of retinopathy can result in vision loss.
The most common presentation of diabetic retinopathy is non-proliferative diabetic retinopathy (NPDR) as it is not a result of new blood vessels, but rather it is due to damage of the patient’s own retinal blood vessels. These vessels become weak and develop small outpouchings called microaneurysms. These microaneurysms leak fluid into the surrounding retina and the resulting retinal swelling can decrease the vision.
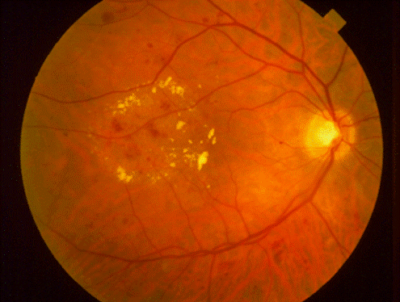
The second and potentially most destructive form of diabetic retinopathy is called proliferative diabetic retinopathy (PDR) which means new unwanted blood vessels begin to grow (proliferate) in the eye. These vessels are believed to grow in an attempt to supply blood to areas of the eye where the blood supply is limited by the diabetic changes in the blood vessels. The new vessels grow haphazardly and often extend into the clear vitreous jelly that fills the back of the eye. Eventually, the vessels can bleed into the eye and cause traction on the retina leading to a detachment of the retina from the back of the eye.

Both proliferative and non-proliferative retinopathy can be treated by laser surgery or injections of medicines into the eye.
Studies have shown that good control of blood sugar and blood pressure can reduce the severity of the disease. We generally recommend our patients strive to keep the Hemoglobin A1C level under 7.0. Even so, there are some patients under reasonably good control who still develop the retinopathy.
Typically, diabetic retinopathy can progress a great deal before the patient notices any visual changes. Furthermore, laser treatment is most effective when performed early in the disease process; therefore, it is very important that all diabetics have a dilated eye exam every year by a professional familiar with the treatment of the disease.
Other Diabetic Eye Problems:
Diabetics can develop eye movement abnormalities due to cranial nerve palsies (palsies are weaknesses). The nerves are believed to have a decreased blood supply due to the diabetes and lose function. Because they control the eye muscles, the eyes can no longer properly align themselves and the patient sees double images. Fortunately, the large majority of these cranial nerve palsies resolve spontaneously over several weeks.
The lens of the eye can be affected in two ways by diabetes. First, wide swings in blood sugar cause the lens to shrink or swell. This change in shape alters how it focuses light onto the retina and thus changes the patient’s refraction (that is their glasses prescription). It is, therefore, usually best to wait until the blood sugar is under control before buying new glasses. The second way diabetes affects the lens is by cataract formation. A cataract is a clouding or discoloration of the clear lens rendering it difficult to see through. Cataract surgery may become necessary when the visual limitation inhibits the individual’s ability to function.
